by James Rakoczi, PhD researcher, Department of English. This post was first published on the Centre for Humanities and Health blog.
On 28 September 2017, the Centre for Humanities and Health brought together a collection of healthcare practitioners, literary scholars, journal editors, teachers and anthropologists at St. Bride’s Foundation off Fleet Street to discuss ambiguities and paradoxes in clinical practice. Because of my research, I spend a lot of my time thinking about ambiguity as it pertains to the experience of being ill, but I rarely get such an opportunity to consider it from the other side—how ambiguity haunts and energises the mechanisms of medical institutions and desires.
The first two papers explored the complexities of quantitative approaches in healthcare. Professor Brian Hurwitz talked us through a recent claim by Jonathan Glass in the BMJ that the ‘plural of anecdote is not data’. It’s not wide off the mark to say that Hurwitz both agreed and disagreed. When we tell an anecdote, we tell it because we consider it worth telling (it might be funny, entertaining or unusual). However, the pedagogic function of anecdote is to illustrate a truth about the world. They recount anomalous events yet, in doing so, reveal regularity. In this, they share an assumption with scientific methodology: the belief that what is true somewhere is true everywhere.
Both anecdote and data has power in this ‘systematicity’: they are embedded in the real. Through an analysis of the importance of anecdote in James Jurin’s 1724-9 study of the inoculation of smallpox – a canonical work in the history of early numerical science – Hurwitz implored us to recognize how data intertwines with the anecdotal. Anecdote cannot expand into data, because anecdote and data relate to one another as, say, different literary genres interrelate.
Seamus O’Mahony, Professor at University College Cork, spoke about the McNamara fallacy:
‘to say that what can’t be easily measured, really doesn’t exist. This is suicide.’[1]
He told a gastroenterological anecdote. In routine colonoscopies, it is considered good practice to detect and remove small, benign growths known as polyps. Gastroenterologists are incentivised to remove polyps in more than 15% of colonoscopies. This led to the death of a man in his mid-80s who contracted an infection after he had a number of polyps removed. Polyps are removed because of the prognostic risk they pose over 10-20 years. Why, O’Mahony asked, was a man’s well-being when he was 105 considered to the expense of his life at 85? The answer: targets. Whatever the efficacy of targets in healthcare, when they are measured only through that which can be measured (i.e., no. of colonoscopies which lead to surgery) then the consequences could be fatal. O’Mahony was careful to distinguish between sincere logical fallacy and deliberately misleading metrical analyses carried out by, say, pharmacological companies.
The next three papers explored how caregiving and illness interrelate. Dr Columba Quigley explored the ambiguities of the good death, generously sharing her own lived experiences as a doctor. Perhaps, she argued, death is just too big for the healthy to comprehend. It is therefore the responsibility of caregivers to recognise that being sick – too close to death – will produce ambiguous desires and discourses which we should not try to incorporate into what we perceive to be more palatable notions, but respect on their own terms.
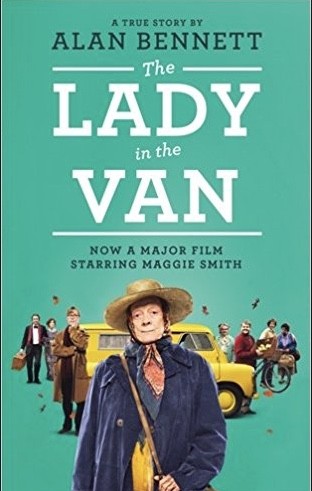
Professor Fergus Shanahan, head of the medical school at University College Cork, delivered a moving paper meditating on the concept of care. He cited Alan Bennett’s Lady in the Van, the story of how Bennett cared for a lady who lived in a van outside his Camden home. Bennett refused, however, to describe care except with disdain.
In Bennett’s account, care is not to be trusted. Care is usually begrudging – a necessary chore. Care is thrust upon you.
Against this account of care, Shanahan discussed shared many accounts he had read, and events he had experienced, of how people turn away from the ill and their relatives. There are numerous examples of this phenomenon in illness memoir but a particularly disturbing example is an essay in which David Rabin, a doctor diagnosed with ALS (Amyotrophic lateral sclerosis), recounts how his colleagues began literally to ignore him. What makes us turn away from rather than turn towards those who need care?
Dr Neil Vickers offered a provocative answer to this paradoxical question: Darwinism. Because long-term illness simply did not exist on the scale it did now (medical advances have extended lifespans), a powerful social text inscribed in the majority of us associates illness with death itself. People instinctively detach themselves from the ill because they understand them as already-dead – a crude reaction predicated by genetic imperatives for survival.
If care is to transcend the un-ethicality of our predispositions, we need to see the life-liness of those associated with death…We must embrace an alternate text, articulated by Albert Robillard: ‘one lives until one dies’.
This symposium was the first of hopefully many collaborations between King’s College London’s English Department and University College Cork. It testified to the interesting things that can happen when an assemblage of people – the likes of which only the medical humanities can bring together – come together under one roof.
[1] Daniel Yankelovich, ‘Corporate Priorities: A continuing study of the new demands on business,’ (Stamford: Daniel Yankelovich, 1972)
You may also like to read
Confessions of a medical humanist
Arabic Illness Narratives and National Politics
Blog posts on King’s English represent the views of the individual authors and neither those of the English Department, nor of King’s College London.