Caroline Emmer De Albuquerque Green, NIHR ARC South London Post-Doctoral Fellow at the NIHR Policy Research Unit in Health and Social Care Workforce, introduces a new report on what Safeguarding Adults Reviews tell us about mental health social care services for adults in London. The report was co-authored with Unit Director Prof Jill Manthorpe and Research Fellow Stephen Martineau. (500 words)
Caroline Emmer De Albuquerque Green, NIHR ARC South London Post-Doctoral Fellow at the NIHR Policy Research Unit in Health and Social Care Workforce, introduces a new report on what Safeguarding Adults Reviews tell us about mental health social care services for adults in London. The report was co-authored with Unit Director Prof Jill Manthorpe and Research Fellow Stephen Martineau. (500 words)
Safeguarding Adult Reviews show that social care can be a matter of life or death when it comes to people experiencing mental health problems. In this new report we focus on a sample of Reviews that bear witness to the sad cases of people who may have been needing or using social care services to support them with mental health problems but who died or had been harmed and where multi-agency working was explored by the Review process. As with all such Reviews, they are designed to help learning and so improve individuals’ care and systems.
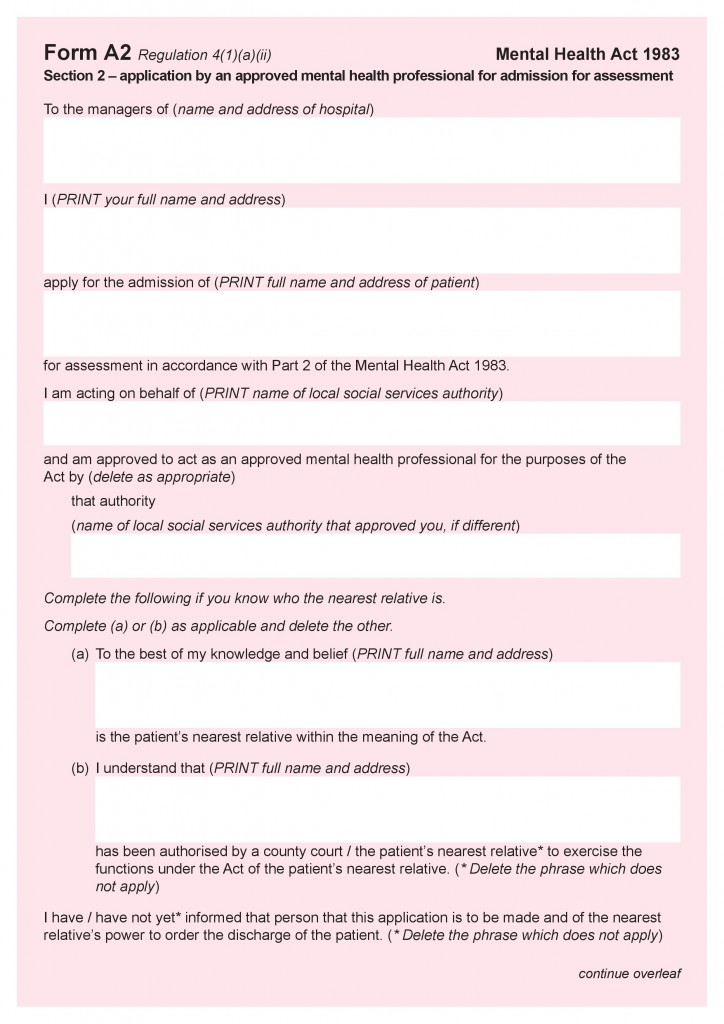
 Our report ‘A matter of life or death: A rapid review assessment of London’s safeguarding adults reviews to inform the future of mental health adult social care under a new Mental Health Act’ was commissioned by LondonADASS (Association of Directors of Adult Social Services). We amplified the learning from Safeguarding Adult Reviews published across all London Councils between 2017 and 2020 and also consulted Coroners’ Reports to Prevent Future Deaths. Our analysis is being used by LondonADASS to inform debates about the proposed new Mental Health Act, where, curiously safeguarding appears to be overlooked. Continue reading
Our report ‘A matter of life or death: A rapid review assessment of London’s safeguarding adults reviews to inform the future of mental health adult social care under a new Mental Health Act’ was commissioned by LondonADASS (Association of Directors of Adult Social Services). We amplified the learning from Safeguarding Adult Reviews published across all London Councils between 2017 and 2020 and also consulted Coroners’ Reports to Prevent Future Deaths. Our analysis is being used by LondonADASS to inform debates about the proposed new Mental Health Act, where, curiously safeguarding appears to be overlooked. Continue reading




 Gaia Cetrano
Gaia Cetrano