 Pay levels, poor awareness of the role, and a lack of associated career benefits all discourage health professionals from training and working as Approved Mental Health Professionals (AMHPs), according to new research by the NIHR Social Care Workforce Research Unit at King’s College London.
Pay levels, poor awareness of the role, and a lack of associated career benefits all discourage health professionals from training and working as Approved Mental Health Professionals (AMHPs), according to new research by the NIHR Social Care Workforce Research Unit at King’s College London.
 Published today, Who wants to be an Approved Mental Health Professional?, finds that closer working between Mental Health Trusts and local authorities, higher remuneration and enhancing the reputation and profile of AMHP work would encourage more health professionals to take up such positions.
Published today, Who wants to be an Approved Mental Health Professional?, finds that closer working between Mental Health Trusts and local authorities, higher remuneration and enhancing the reputation and profile of AMHP work would encourage more health professionals to take up such positions.
Greater engagement from the Royal Colleges of Nursing and Occupational Therapists, and the Nursing and Midwifery Council, may also make the AMHP role more attractive by helping to embed it in these health professionals’ career plans.
The research highlights how organisational barriers – such as difficulties in managing AMHPs across separate local authority and mental health trust teams – deter many health professionals from taking up the role.
The study consists of more than 50 interviews with individuals involved in AMHP services, as well as a survey of Local Authority AMHP Leads.
 Unsurprisingly, health professionals interviewed for the research reported needing a high degree of motivation to become AMHPs, often having to overcome opposition from their managers. Some also feared being responsible for decisions to detain patients, which they thought would make it more difficult for them to establish and maintain therapeutic relationships.
Unsurprisingly, health professionals interviewed for the research reported needing a high degree of motivation to become AMHPs, often having to overcome opposition from their managers. Some also feared being responsible for decisions to detain patients, which they thought would make it more difficult for them to establish and maintain therapeutic relationships.
Although the immediate nature of AMHP work, including crisis resolution, makes it attractive to many health professionals, the difficulty of arranging effective supervision was another challenge highlighted.
 Despite the barriers, most participants were positive about health professionals’ ability to work effectively as AMHPs.
Despite the barriers, most participants were positive about health professionals’ ability to work effectively as AMHPs.
However, local authorities and NHS Mental Health Trusts were increasingly focusing on ‘core business’, which may mean the NHS is less enthusiastic about supporting health staff to become AMHPs, as the AMHP service is a local authority responsibility.
AMHPs are responsible for deciding, with the advice of two medical doctors, whether a person assessed under the Mental Health Act 1983 should be compulsorily admitted to hospital (also known as ‘sectioning’).
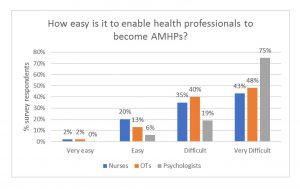 There is currently a shortage of AMHPs at a time when the number of Mental Health Act assessments is increasing. 95% of AMHPs are social workers, highlighting the need to recruit more health workers to the role. One of our main findings was that AMHP Leads regard it as difficult to enable health professionals to become AMHPs.
There is currently a shortage of AMHPs at a time when the number of Mental Health Act assessments is increasing. 95% of AMHPs are social workers, highlighting the need to recruit more health workers to the role. One of our main findings was that AMHP Leads regard it as difficult to enable health professionals to become AMHPs.
This research stresses the importance of local authorities and Mental Health Trusts committing to working together to encourage and support health professionals to become AMHPs. At a time of pressure on public services, it is natural that they focus on ‘core business’, so it will be important to ensure that the AMHP service is not seen purely as a local authority responsibility by all agencies involved.
The research has been welcomed by Lyn Romeo, Chief Social Worker for Adults, ‘I have asked my team to work with Health Education England, Social Work England and the Association of Directors of Social Services to ensure that we use this very helpful and timely research from the NIHR Social Care Workforce Research Unit to develop our workforce plan for Approved Mental Health Professionals so that we can encourage all relevant professionals to train to be AMHPs.’
We made these suggestions for overcoming barriers to health professionals becoming AMHPs, which we hope will be useful for the Independent Mental Health Act Review:
- Give Local Authorities specific responsibilities to enable and fund health professionals working for Mental Health Trusts to take up AMHP training (which may require extra funding for Local Authorities)
- Increase the amount paid to AMHPs
- Make nationwide decisions about the amount to pay AMHPs and how to pay them
- Equate AMHP pay with enhancements for other clinical nurse specialisms (e.g. nurse prescriber)
- Engage with professional bodies, such as the Royal College of Nursing and Royal College of Occupational Therapists and regulators such as the Nursing & Midwifery Council. This would help foster greater confidence that becoming an AMHP is an important and rewarding means of career advancement for these health professionals.
The report (and a summary report) is available from the project page:
Stevens, M., Martineau, S., Manthorpe, J., Steils, N. and Norrie, C. (2018) ‘Who wants to be an Approved Mental Health Professional?’ London: Social Care Workforce Research Unit, King’s College London.