This post was written by Charlotte Kelley Jones. Charlotte is a postgraduate research (PGR) student within the Faculty of Life Sciences & Medicine and School of Cancer & Pharmaceutical Sciences. She works in the Cancer Behavioural Science Group within the King’s Cancer Prevention Group. Charlotte has a background in behavioural science and health psychology. Her doctoral research focuses on the acceptability of incorporating risk stratification within the NHS Breast Screening Programme.
Screening programmes generally change because the evidence about screening changes. The NHS breast screening programme (NHSBSP), which invites all women for mammography screening aged between 50 and 70 years on a triennial basis, is now more than thirty years old. Although evidence suggests an affirmative response to the question of whether “mammography screening is still worthwhile?”, the NHSBSP is not currently aligned with advances in epidemiological and aetiological knowledge about breast cancer.
Increased ability to predict the risk of breast cancer.
Over the past 3 decades, researchers have identified breast cancer risk factors additional to age and gender: e.g., polygenic risk, family history, lifestyle, hormonal and reproductive history. Furthermore, the development of and validation of multifactorial breast cancer risk prediction models such as the Tyrer-Cuzick model and the Breast and Ovarian Analysis of Disease Incidence and Carrier Estimation Algorithm (BOADICEA), are increasing the clinical feasibility of introducing personalised risk-stratification within the NHSBSP in time.
What would a risk-stratified NHS breast screening programme look like?
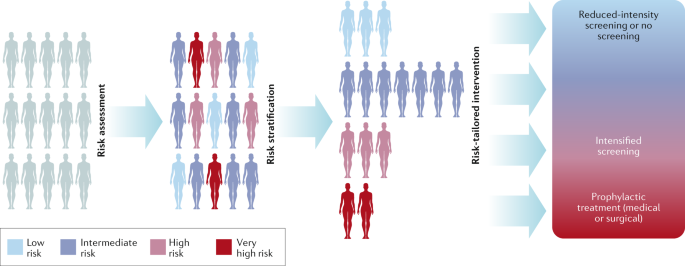
The assessment of individual risk factors to calculate personalised risk scores will enable the classification of women into risk groups. Consequently, screening frequency, test modality, and/or age range of screening eligibility could be adjusted to potentially optimise the benefit to harm ratio of breast screening specific to the level of risk. In other words, reducing the potential for harm of over-diagnosis and the psychological distress of false-positive results whilst maintaining the benefits of early detection. Furthermore, preventative and risk-management opportunities would be integrated within this screening infrastructure enabling women to actively reduce their breast cancer risk through health behaviour change and/or chemoprevention.
The role of behavioural science for assessing the feasibility of risk-stratified breast screening.
Implementing changes to an established national cancer screening policy can be controversial and more challenging than introducing a new screening programme. A case in point is the widespread opposition to changes in USA breast screening guidance which served to highlight the need for clear and consistent communication. Nevertheless, in terms of ensuring the effectiveness of health screening interventions, policymakers now acknowledge that identifying what matters to stakeholders may be of equal importance as the evidence for clinical utility. Consequently, there is a growing focus on behavioural and social science research to better understand the interpersonal and sociocultural contexts shaping public screening preferences.
Recently, acceptability has become a key consideration in the design, evaluation, and implementation of healthcare interventions. Poor levels of acceptability born of a failure to communicate effectively with the screening population can undermine public confidence. For instance, a missed opportunity to clearly communicate proposed changes to screening intervals (2 to 5-years) and test modality (Pap smears to HPV testing) within the Australian National Cervical Screening Programme contributed to considerable public opposition which seemed to stem from a lack of knowledge and misconceptions about the reasons behind the changes as a form of reducing healthcare costs.
Therefore, Charlotte Kelley Jones and Jo Waller (Behavioural Science Team, Cancer Prevention Group) with Suzanne Scott (Oral, Clinical & Translational Sciences) are currently investigating whether women consider the incorporation of risk-stratification within the NHS breast screening programme prospectively acceptable, in a project funded by Breast Cancer Now. This is important as changes to the current ‘one-size fits all’ nature of the NHSBSP by the introduction of risk-based screening recommendations may be perceived as unequitable or as rationing of health care provision. Moreover, this approach will bring the importance of informed screening decision-making into sharp focus and necessitate improving lay understanding of breast cancer risk and screening-related harms. Consequently, behavioural scientists have a vital role to play in ensuring clear communication of the rationale for risk-stratified breast screening and understanding women’s prospective preferences for this approach.
This project will use a range of methodologies, including interviews, a discrete choice experiment and a population-level survey, to provide a comprehensive assessment of UK women’s anticipated cognitive and emotional responses to the prospect of introducing risk-stratification within the NHSBSP. We believe that this broad perspective will help to bridge the gap between clinical research and future breast screening practice.
We will keep you posted about UK women’s thoughts and feelings towards the prospect of a risk-stratified NHS breast screening programme in a future blog.
Share this Page

Leave a Reply