 Dr Nathan Davies discusses Rules of Thumb for End of Life Care for People with Dementia. (954 words)
Dr Nathan Davies discusses Rules of Thumb for End of Life Care for People with Dementia. (954 words)
Back in 2011 when I started my PhD and was working on a European study which was examining palliative care services for people with dementia, there was a distinct lack of guidance about how end of life care should be delivered. The only real ‘saving grace’ I guess was the Liverpool Care Pathway. This offered some guidance about what should happen towards the end of life. It was meant to incorporate and describe best practice from hospice care, the ‘gold standard’ of end of life care, and allow it to be translated to other settings such as the acute hospital ward. Although, I say saving grace… really, it wasn’t best suited to people with dementia and it only focused on the last few days of life.
The Liverpool Care Pathway received some shocking criticism, spearheaded mainly by the Daily Mail and ultimately this led to the removal of the pathway by the UK government in 2013. What we saw in the middle of our projects were practitioners losing more and more confidence in providing end of life care generally, let alone for people with dementia.
This led us to think, what can we do to help with practitioners confidence but not develop yet another pathway or guideline? Maybe what we need is something that is short, easy to remember, prompts us to think and leads us to an action. Cue light bulb moment, and we have the idea of developing rules-of-thumb (heuristics). Rules-of-thumb are simple, easy to remember schematic patterns which help with decision making. We were fortunate to gain funding for this research from the Alzheimer’s Society and Marie Curie. Our research team included dementia and end of life care experts, including Prof Steve Iliffe, Dr Kethakie Lamahewa, Prof Jill Manthorpe, Dr Rammya Mathew, and Dr Liz Sampson.
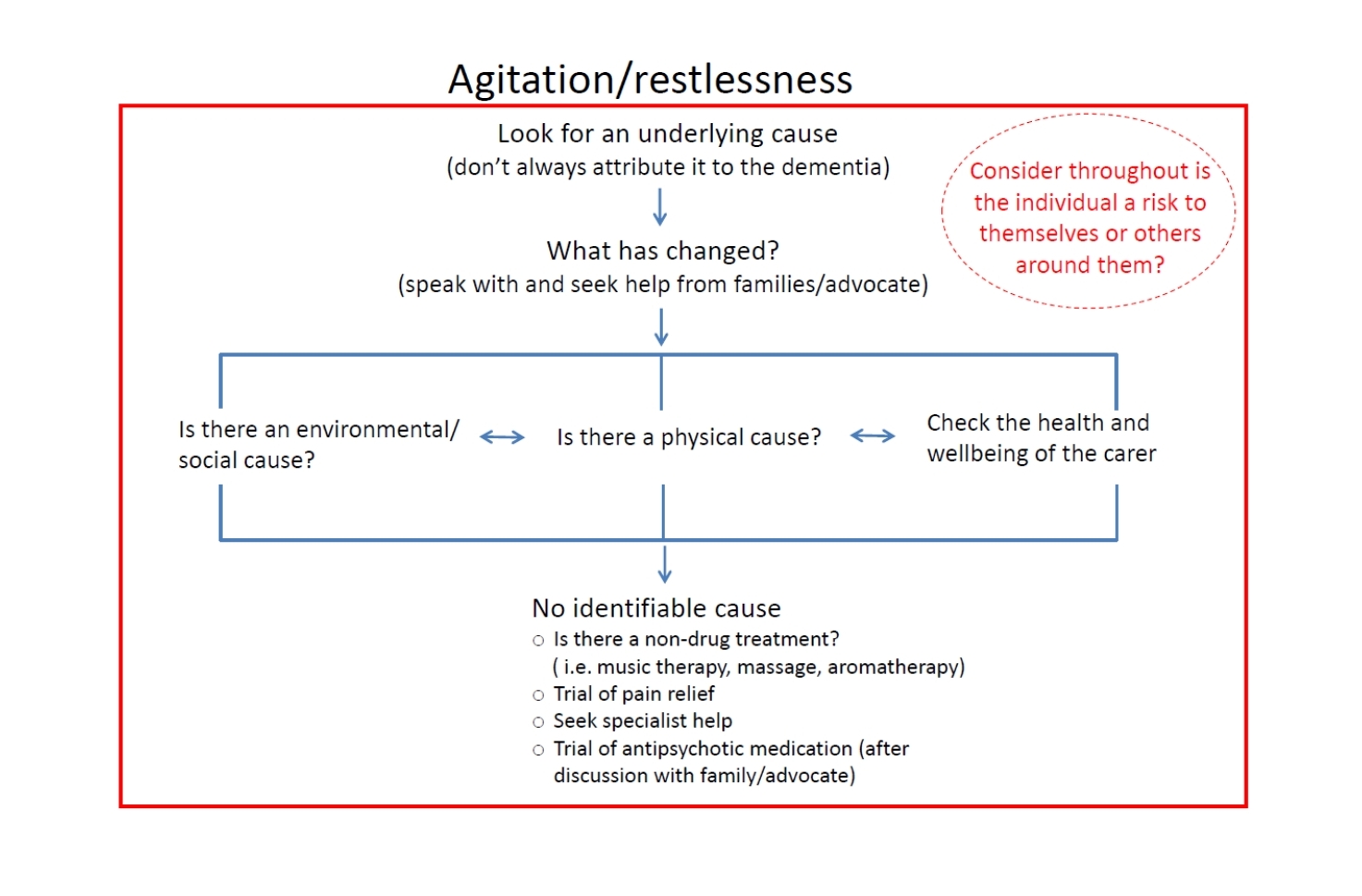
Could we produce something similar to this for practitioners making decisions for people with dementia at the end of life? Well, using a process of continual development and change with families and practitioners, we did. We have produced four rules-of-thumb, covering: eating and swallowing difficulties; agitation and restlessness; reviewing treatment and interventions at the end of life; and providing routine care at the end of life.
The full rules are available here. But to give you a taster our rules consist of flow charts, taking the decision maker, through the thought processes and the individual smaller thoughts and decisions which need to be made about a much larger decision. In the diagram you can see our rule covering agitation and restlessness. The key rule here is to not assume that the dementia is the cause of the agitation/restlessness, but to look for an underlying cause. It also acts as a prompt to the practitioner, getting them to think; what else is going on here? They need to look at the changes that have occurred, thinking not only about the physical causes, but also the environment and the health and wellbeing of the carer. Finally, this rule reassures the practitioner that a cause may not always be found. This is ok!
We tested these rules at 5 different sites; 2 palliative care teams, a community nursing team, a general practice, and a hospital ward. In September we hosted the end of study symposium to present the final versions and hear some feedback from those on the ground who actually used them.
Gillian Green, a community matron, said they were easy to follow providing common sense advice and she had not seen anything quite like it in her 26 years of experience in nursing.
Caroline Ashton, who has just gained her Master’s in Advanced Dementia Care and undertook her dissertation at SCWRU, also fed back on her experiences of using the rules-of-thumb on her complex care hospital ward. She told the audience about how a locum registrar (doctor) on the ward was able to pick up the rules-of-thumb to help guide decisions about a patient, despite having very little experience of end of life care. That registrar has taken the rules away with her to use in her clinical practice.
The feedback we had from sites through our evaluation was great, with suggestions for improvement incorporated into a final toolkit of the rules-of-thumb. We are in the process of analysing the final evaluations and will publish these findings in more detail very soon.
So are rules of thumb the answer? I won’t say yes, but I definitely will not say no! Our experiences is that they have been a good way to get practitioners thinking about some of the basic underpinnings of end of life care, making the implicit knowledge that they have explicit. We have provided many of those involved in the study with copies of the final rules-of-thumb for them to not only continue using in practice but also to share within their wider organisations and colleagues. As I sit writing this blog I have opened another email explaining how the rules-of-thumb we have developed are going to be incorporated into end of life training being developed by the Alzheimer’s Society.
For more information on our work please see our papers below or contact Dr Nathan Davies (Nathan.davies.10@ucl.ac.uk)