When you first think of taxonomy, you might consider biology lessons and branches of the evolutionary tree: a hierarchy from a seaweed to a rose, 18th century botanical drawings, colorful wings of different species of butterflies filed away in museum cabinets. Psychiatry is unlikely to come to your mind, yet it is the classification of mental disorders that is currently undergoing a revolution.

Traditional classification of psychopathology is specified in manuals such as the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) [1]. Diagnostic manuals are important because they guide diagnosis of mental illness, which in turn informs patient treatment, guides research efforts, and is used by drug companies to develop new medications.
Limitations of traditional classification systems are widely acknowledged and discussed [2-4]. They include arbitrary boundaries between psychopathology and normality, diagnostic instability, and inability to account for subthreshold cases. To address them, an international consortium of over 50 psychologists and psychiatrists has recently published the Hierarchical Taxonomy of Psychopathology (HiTOP), a dimensional classification system of a wide range of psychiatric problems, developed to reflect the state-of-the art scientific evidence [5]. This and similar efforts are likely to change the classification and diagnostic practices in psychiatry in the future.
“It is the function of science to discover the existence of a general reign of order in nature and to find the causes governing this order. And this refers in equal measure to the relations of man – social and political – and to the entire universe as a whole.”
― Dmitri Mendeleev, the author of the Periodic Table of Elements
Structure of Emotional Disorders
Emotional problems, such as depression and different types of anxiety, co-occur more frequently than expected by chance, with most patients labelled with more than one emotional disorder at the same time. Furthermore, some diagnoses are so complex that often two patients with the same diagnosis share very few symptoms in common. For example, depression is characterized by numerous cognitive and physiological symptoms, such as low mood, loss of pleasure, insomnia, lack of energy, suicidality, change in appetite…the list goes on! These two issues – comorbidity between the disorders, and heterogeneity within them – clearly illustrate that for emotional problems, diagnostic categories are imperfect.
With the aim to better classify emotional disorder symptoms, my collaborators and I recently analyzed data from two large samples of outpatients and students with a history of mental health illness [6]. Participants were interviewed about their experiences of a whole range of emotional symptoms underpinning depressive, bipolar and anxiety disorders as well as post-traumatic stress disorder (PTSD) and obsessive–compulsive disorder (OCD). Using data on individual symptoms, we simultaneously mapped out the structure of emotional disorders at several levels of the hierarchy, describing which symptoms cluster together into tight-knit lower-order dimensions, as well as more broadly into higher-order spectra. Such hierarchical approach accounts for comorbidity, and allows to describe mental illness with the desired degree of specificity, explicating heterogeneity within disorders.
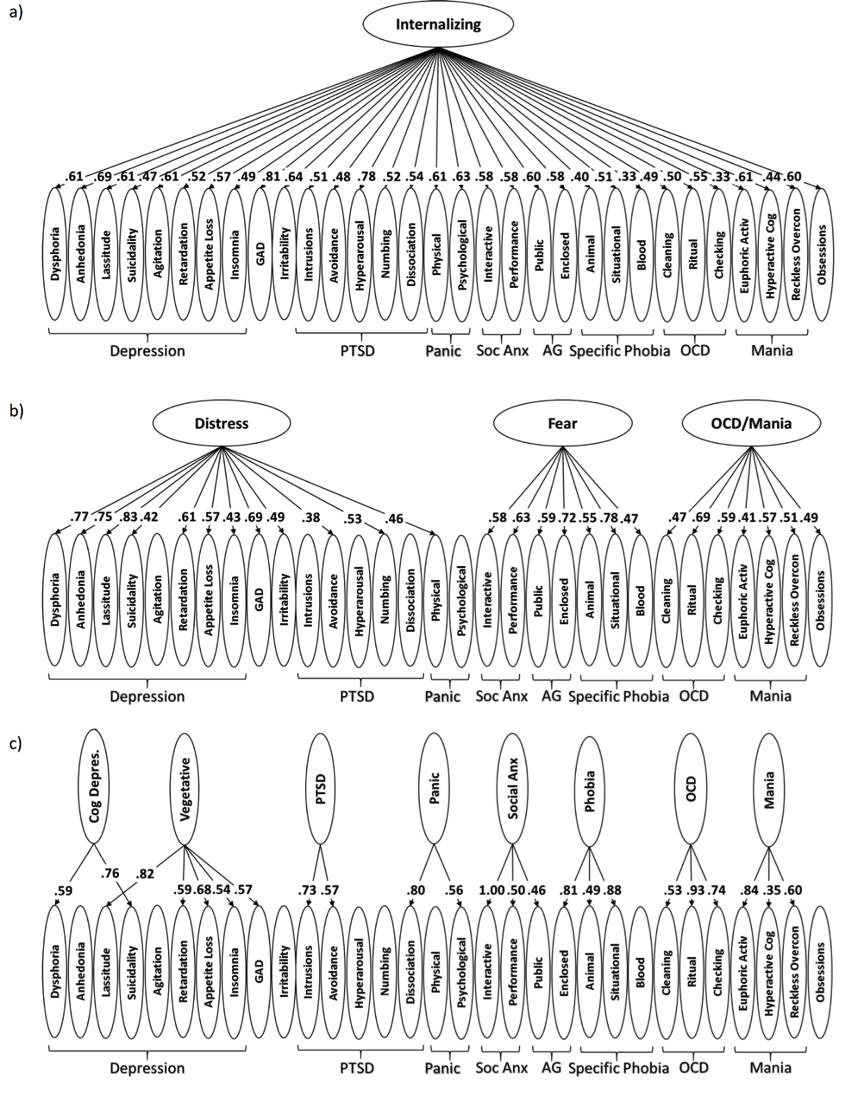
The resulting structure of emotional disorders is presented in Figure 1. As expected, we found that most diagnoses were heterogenous and consisted of numerous narrow components. For example, within the agoraphobia diagnosis, fears of public spaces were separate from fears of enclosure. At the intermediate level of hierarchy, narrow components often clustered in a way that did not adhere to diagnostic boundaries. For example, agoraphobia’s fear of public spaces was linked to social anxiety, while the fears of enclosure were most closely associated with symptoms of specific phobias. Similarly, eight depressi on components divided into separate cognitive and vegetative (physiological) syndromes. At an even higher level of the hierarchical structure, we observed that emotional problems clustered into Distress, Fear and OCD/Mania spectra, in line with a large body of literature supporting this division of emotional psychopathology [7, 8]. We have also demonstrated that these problems belong to an overarching Internalizing spectrum.
on components divided into separate cognitive and vegetative (physiological) syndromes. At an even higher level of the hierarchical structure, we observed that emotional problems clustered into Distress, Fear and OCD/Mania spectra, in line with a large body of literature supporting this division of emotional psychopathology [7, 8]. We have also demonstrated that these problems belong to an overarching Internalizing spectrum.
Overall, the evidence-based, symptom-driven structure differed from how the DSM-5 conceptualizes emotional disorders. Future work should extend the structure to encompass other forms of Internalizing psychopathology, such as eating disorders and sexual problems. It would be also fascinating to test whether the structure replicates in children and adolescents.
Taxonomy in Clinical Setting
The obvious next step is to ask whether the new classification improves on categorical diagnoses in accounting for consequential outcomes, such as functional impairment. Indeed, this is what we found –information contained in the hierarchical classification was about twice as good at predicting patients’ overall functioning as DSM diagnoses. This is remarkable given that functional impairment is explicitly included in diagnoses, but not in the symptom assessment.
Following up on this finding, in another set of analyses we explored whether the derived structure of emotional disorders can account for naturalistic medication prescription patterns better than traditional diagnoses [9]. We found that narrow dimensions underpinning diagnoses were linked to different medication prescriptions. For example, in patients with depression, dysphoria and anhedonia symptoms were associated with prescription of antidepressants and anxiolytics, while insomnia was associated with prescription of hypnotic medications. Furthermore, clinicians often prescribed the same psychiatric medication for a wide range of diagnoses. Overall, symptom dimensions predicted the pattern of medication prescription better than DSM diagnoses, suggesting that it is the specific symptoms that guide clinicians’ decision making. Thus, the empirical classification of symptoms may be a more effective guide to pharmacotherapy than traditional diagnoses.
In sum, classification of emotional disorders matters in clinical setting. A well characterized cluster of symptoms at the lower level of hierarchy can provide good targets for symptom-specific treatments, e.g., exposure therapy for specific phobia. The higher level of hierarchy is helpful when designing comprehensive treatment packages and developing public health policy. For example, risk factors such as childhood abuse are not specific to one diagnosis [10, 11], suggesting that targeting these higher-order risk factors may have the broadest impact.
Figure 1 – Hierarchical Structure of Emotional Disorders.
Note: Numbers reflect factor analytic loadings. For full results, see [6].
PTSD-posttraumatic stress disorder; Soc Anx–social anxiety; AG–agoraphobia; OCD-obsessive-compulsive disorder; Cog Depress–cognitive depression.
Dr. Monika Waszczuk PhD, Stony Brook University School of Medicine
Acknowledgement: Many ideas and thoughts in this post are inspired Dr. Kotov, the founder of the HiTOP consortium and my supervisor on classification projects.
References
- American Psychiatric Association, Diagnostic and statistical manual of mental disorders, DSM-5. Fifth ed. 2013, Arlington, VA: American Psychiatric Publishing.
- Insel, T., et al., Research domain criteria (RDoC): toward a new classification framework for research on mental disorders. American Journal of Psychiatry, 2010. 167(7): p. 748-751.
- Clark, L.A., D. Watson, and S. Reynolds, Diagnosis and classification of psychopathology: Challenges to the current system and future directions. Annual review of psychology, 1995. 46(1): p. 121-153.
- Zimmerman, M., et al., How many different ways do patients meet the diagnostic criteria for major depressive disorder? Comprehensive psychiatry, 2015. 56: p. 29-34.
- Kotov, R., et al., The Hierarchical Taxonomy Of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of abnormal psychology, 2017. 216(4): p. 454.
- Waszczuk, M.A., et al., Hierarchical Structure of Emotional Disorders: From Individual Symptoms to the Spectrum Journal of Abnormal Psychology, 2017.
- Watson, D., Rethinking the Mood and Anxiety Disorders: A Quantitative Hierarchical Model for DSM–V. Journal of Abnormal Psychology, 2005. 114(4): p. 522-536.
- Forbush, K. and D. Watson, The structure of common and uncommon mental disorders. Psychological medicine, 2013. 43(01): p. 97-108.
- Waszczuk, M.A., et al., What do clinicians treat: diagnoses or symptoms? The incremental validity of a symptom-based, dimensional characterization of emotional disorders in predicting medication prescription patterns. Comprehensive Psychiatry, 2017.
- Vachon, D.D., et al., Assessment of the Harmful Psychiatric and Behavioral Effects of Different Forms of Child Maltreatment. JAMA psychiatry, 2015: p. 1135-1142.
- Keyes, K.M., et al., Childhood maltreatment and the structure of common psychiatric disorders. The British Journal of Psychiatry, 2012. 200(2): p. 107-115.