
By Cristina Fernandez, research assistant, King’s College London
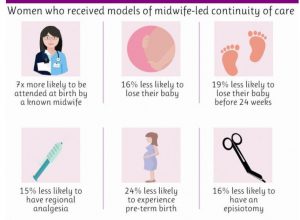
Increasing midwifery continuity of care has been identified as a key priority for maternity services in the United Kingdom (UK). A Cochrane review led by Professor Sandall and colleagues found that women who receive care by one named midwife or a small group of midwives throughout pregnancy, birth and postnatal periods are 24% less likely to experience a preterm birth and more likely to have better maternal and infant outcomes, have more positive experiences of care and use resources more effectively. This is particularly important considering increasing rates of preterm births worldwide and their adverse infant outcomes in terms of survival, quality of life, psychosocial impact on the family and costs to society.
The ongoing POPPIE trial (Pilot Study of midwifery Practice in Preterm birth Including women’s Experiences) is investigating whether a model of midwifery continuity of care for women at increased risk of preterm birth is feasible and improves experience and pregnancy outcomes in a hospital in south London. To develop and implement this complex organisational intervention, we used the IMPRES tool and took a collaborative approach involving many stakeholders from the NIHR CLAHRC South London, King’s College London, Lewisham Clinical Commissioning Group, London Borough of Lewisham, the Maternity Voices Partnership (MVP), parents of preterm babies (including fathers); and other service-user organisation representatives and charities (e.g. BLISS, Tommy’s charity).
We used numerous strategies to guide the implementation, including applications for funding; involvement of executive boards; business cases; quarterly updates on progress; newsletters; regular implementation meetings; seminars, training and events e.g. the Continuity of Care Study Morning and the POPPIE trial launch, where local commissioners highlighted:
“We are very proud to be part of this exciting collaboration, which is an example of true partnership working… We have high hopes for the learning that will be generated from the trial in terms of improving support for women at risk of pre-term birth, as well as for other women accessing the maternity services…”.
Public health specialists stressed that “a commitment is needed to make continuity of midwifery care work. It is so important, specially for more vulnerable women…”. And an MVP member and mother of a preterm baby crystalised what it means for babies and their families when they are born very early. She added “I’m most pleasantly surprised by POPPIE… What a sensible and forward-thinking way to track the very big problem of preterm birth”. On November 2017, POPPIE won the Know your CLAHRC Award for the Most Innovation Collaboration as part of the maternity and women’s health theme. The judge said: “This is an excellence example of collaboration with extensive set of stakeholders spanning the voluntary sector, commissioners, NHS organisations, parents and academia”.
A total of 332 women have been included in the pilot trial up to date and recruitment is due to be completed by the end September. Some of the midwives shared their views on the POPPIE team: “Since the beginning I have always known how important POPPIE is and providing continuity of care…I love my women calling me by my name before stepping in their houses…”. Another midwife emphasised “It was so lovely to be with Tash for the delivery of her 4th baby (and first baby of the trial!), which came earlier than expected… I think she appreciated that we now know each other well and the extra support this gives”.
We have shared experiences of developing and implementing this pilot trial at national and international workshops, seminars and conferences in the UK, United States and Australia. In December 2017, a group of Swedish midwives developing a midwifery continuity of care model, visited the POPPIE team and discussed the philosophy of the model, how they work as part of the team; how they organise the workload; how they ensure 24 hour cover for women in labour, etc. In April 2018, I had the opportunity to visit Australia as part of a Florence Nightingale Foundation Travel Scholarship Award. I met researchers, public health specialists, clinicians and midwives in Sydney, Brisbane, Melbourne and Alice Springs in the Northern Territory to share experiences from POPPIE and explore public health models of maternity care for the Indigenous community.

And very recently, Prof Øvretveit and Dr Ahlberg from Karolinska Institute visited the research team at King’s College London to explore practical issues in implementation of continuity of care models for vulnerable and immigrant women.
Midwifery continuity of care of care has lately got much attention in policy developments in the UK and internationally. Continuity of care is mentioned in the WHO recommendations for antenatal care for a positive pregnancy experience as part of the health systems interventions to improve utilisation and quality of antenatal care. WHO statement on World Prematurity Day focused on midwifery continuity of care, Kangaroo Mother Care and key specific clinical interventions (e.g. antenatal corticosteroids; magnesium sulphate for fetal neuroprotection). In the UK, a new maternity strategy to reduce the number of stillbirths was presented by Health and Social Care Secretary, Jeremy Hunt in November 2017 bringing together many important actions (e.g. independent investigations) and citing the importance of continuity of midwife care as a safety net. In March 2018, new government plans announced an extra 3,000 midwives over the next four years and promised ‘continuity of carers’ by 2021. Our project will allow us to reflect and evaluate the progress and quality of implementation of a midwifery continuity of care model. It will also, however, help us to understand mechanisms of impact on maternal physical, psychosocial, neonatal health, and women’s experiences of care, quality of care and resource use.

Leave a Reply