
The NHS Bowel Cancer Screening programme is on track to meet its objective of reducing deaths from bowel cancer. Our recently published study, the first to evaluate the impact of the bowel screening programme in England found that people who participate in screening reduce their risk of dying from bowel cancer by about 16%.
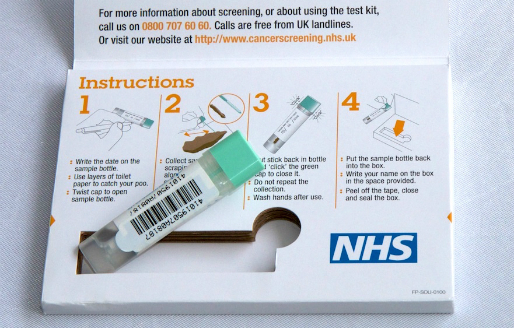
Our study evaluated the impact of the first few years of gFOBT (guaiac faecal occult blood test) screening in England. The aim of gFOBT screening is to diagnose bowel cancer at an early stage, thereby increasing the likelihood that treatment will be successful and prevent death. Early stage bowel cancer can be difficult to detect, as it may not cause symptoms, which is why screening is essential. When diagnosed at its earliest stage, more than 9 in 10 (92%) people with bowel cancer will survive their disease for five years or more, compared with 1 in 10 (10%) people when the disease is diagnosed at the latest stage. Indeed, the tragic death of Dame Deborah James, at the tender age of 40, has raised public awareness about this cancer.

As expected, our study found that people who participated in bowel screening were roughly at the same risk of being diagnosed with bowel cancer as people who did not get a screen. Importantly this result suggests that screening is not actually diagnosing bowel cancers that would never have caused symptoms or problems.

However we found that individuals who participated in screening reduced their risk of developing advanced stage bowel cancer by around 30%.
This links in with another of our findings that people with advanced bowel cancer were much less likely to participate in screening when compared to people without bowel cancer.
It has long been thought that individuals who accept the invitation to screening (participants) may have a priori better health compared with individuals who do not (non participants). In the case of bowel screening, a previous study found that the screening kit return rate was lower for postcode areas associated with poorer health status. Therefore, even without any benefit of screening, those who would participate in screening may be less likely to be diagnosed with advanced bowel cancer compared with the general population. This is often referred to as self-selection bias. In this study we were careful to account for this in the analysis.
The Faecal Immunochemical Test (FIT) was launched on 20th November 2017, replacing the Faecal Occult Blood Test (FOBT). This is a more sensitive test therefore the benefits of screening in terms of prevention of late-stage disease and mortality are likely to be larger in the future.
Bowel screening using the FIT test is currently offered to individuals aged 60 to 74 years.
Although the test type has been changed our conclusions are still relevant and every effort should be made to increase participation of eligible individuals and particularly to engage those with poor health or living in deprived areas.
The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorse those views or opinions.

Leave a Reply