
This post was created by Amy Tickle, a Cancer Research UK-funded PhD student in the Cancer Prevention Group. Amy is currently in her second year of her PhD and is supervised by Professor Peter Sasieni. Prior to starting her PhD at King’s, Amy completed her MSc in Epidemiology at Imperial College London, where she gained research experience in cancer epidemiology and prevention. In this blog post she discusses the focus of her PhD project and the motivation behind it.
First of all, here is a 2 minute intro video where Amy summaries 3 challenges to consider when monitoring progress in early diagnosis…

Monitoring improvements in early diagnosis
Past research has estimated that 10,000 lives could be saved each year if English survival rates were raised to the best rates in Europe. This estimation could be made possible by reducing the rate of cancers diagnosed at a late stage, i.e., those cancers diagnosed at either stage 3 or 4. By diagnosing cancer earlier, we can increase the opportunities available for curative treatment and in turn, reduce mortality. In this blog post, I will discuss how my PhD research aims to contribute to answering the question “How should we monitor progress in early diagnosis?”
Diagnosing 75% of cases at an ‘early stage’ by 2028
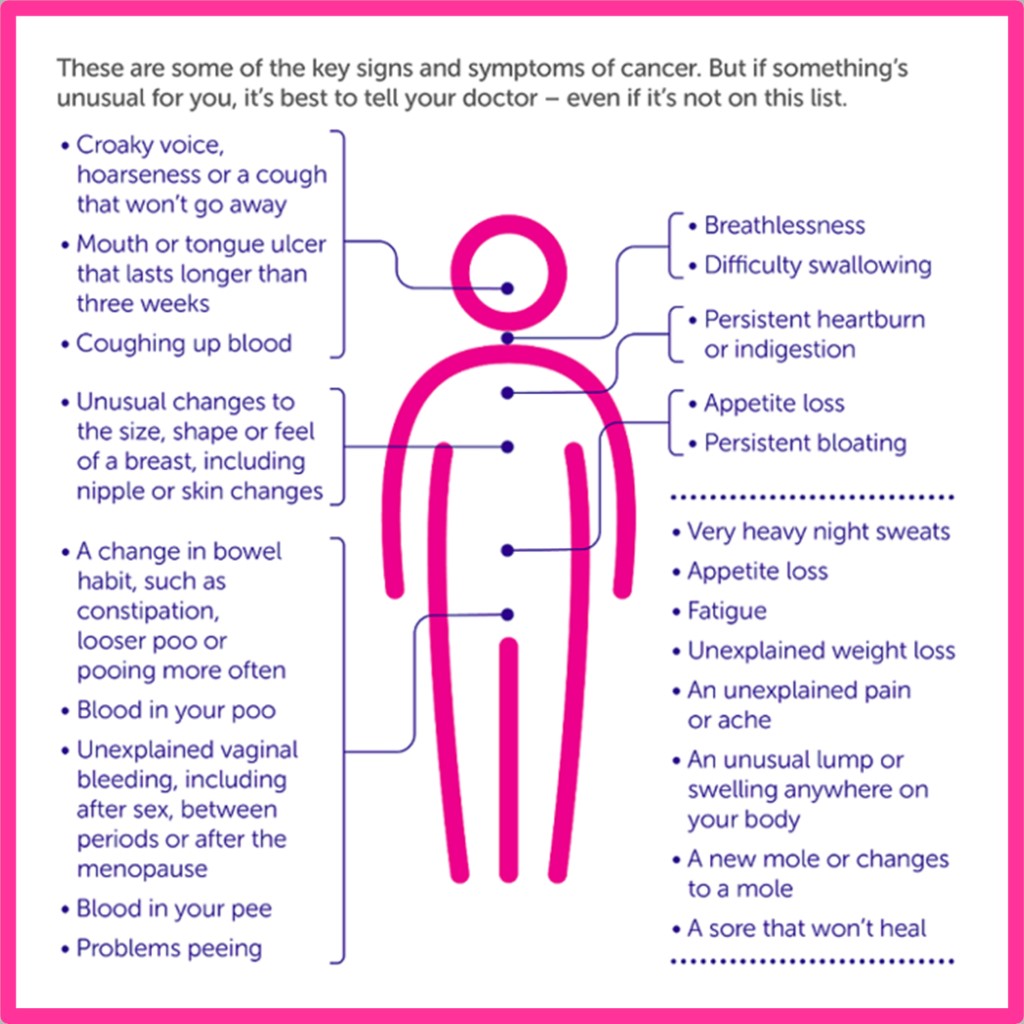
Improving early cancer diagnosis has been an important focus in England during recent years, with 2 key goals being set in the last 8 years to improve early diagnosis and cancer survival. The first was set by Cancer Research UK (CRUK) in 2014 and aimed to see 75% of people surviving with cancer for 10 years or more by 2034. The second, set as part of the NHS’ Long-Term Plan in 2019, aimed to diagnose 3 in 4 cancers at an early stage by 2028. The term ‘early stage cancer’ refers to cancer diagnosed at either stage 1 or 2. Numerous initiatives have been introduced to help meet these goals; these include screening programmes, symptom awareness campaigns and changes to diagnostic pathways. Currently, there are national screening programmes in England for 3 cancer sites: breast, bowel and cervical cancer. These programmes aim to detect pre-cancer or early-stage cancer in asymptomatic individuals, with the hope of offering earlier intervention and treatment. Symptom awareness campaigns include the Be Clear on Cancer campaigns, which ran from 2012 and encouraged people with symptoms to see their GP without delay through multiple media platforms. These screening programmes, awareness campaigns and any other initiatives need to be carefully monitored using metrics along the patient pathway, to assess whether they are on target to meet their overall goal of reduced cancer mortality.
Source: Cancer Research UK
A combination of measures is needed
The evaluation of the success of early diagnosis initiatives requires a combination of both process measures and outcome measures. Outcome measures refer to the clinical outcomes which reflect the impact of an intervention on the patient, for example mortality, to demonstrate whether the overall aims are being achieved. In contrast, process measures refer to the specific steps in an intervention that lead to an outcome, for example cancer screening attendance. Process measures measure how well a service is being delivered. Whilst outcome measures are essential for understanding the direct impact of early diagnosis initiatives on late-stage cancer rates and survival, they cannot be measured for some time. This lag time has been demonstrated in numerous historic clinical trials investigating the impact of breast screening on breast cancer mortality. The findings of such studies demonstrate the need to monitor process measures alongside outcome measures, to provide an early indication of intervention success before outcome data is available.
Process measures may be able to predict outcome measures
Currently, there is very little evidence in the literature investigating associations between process measures and outcome measures. However, if associations are present, process metrics may be able to predict cancer outcomes. These measures are specific to individual interventions; in a breast screening context, process measures would include the proportion of women eligible for screening who received a technically adequate screen (uptake) and the percentage of screened women referred for further assessment (referral rate). Monitoring these process measures could help to assess whether we are making improvements in early diagnosis, by helping to predict how advanced-stage cancer rates will be impacted in several years time.

Difficulties with monitoring true progress in early diagnosis
Despite the range of metrics available, monitoring true progress in early cancer diagnosis can be challenging (3 of which I explain in the accompanying video!).
Several biases exist, including overdiagnosis – the diagnosis of cancers that would never have become clinically significant, and lead-time bias – the inflation of survival time due to earlier diagnosis by screening, despite the patient not living any longer. These biases add to the difficulties of monitoring progress in early diagnosis. Additionally, each individual metric has further drawbacks. Calculating survival is often made difficult by incomplete data within cancer diagnosis registries i.e. staging of the cancer, whilst mortality rates are impacted by inaccuracies in the recording of cause of death. Therefore, further research into the best metrics and indicators for monitoring progress in early diagnosis is needed.
Therefore, my PhD uses a variety of methods to identify the best metrics for monitoring progress in early cancer diagnosis. So far, this research question has been investigated in two separate projects; the first focusing on evaluating breast screening programmes and the second focusing on evaluating the Bowel Be Clear on Cancer campaign. The first project aims to determine the best metrics for monitoring the impact of breast screening programmes, including new, potential measures to improve the current evaluation, using interviews and focus group with experts from a variety of disciplines. These disciplines included breast screening, cancer screening, health economics and engineering. The second project aims to use statistical methodology to identify the best metrics from the Be Clear on Cancer campaign for predicting late-stage bowel cancer rates and bowel cancer survival rates. Overall, the key aims of my research are to identify the most appropriate metrics for highlighting early diagnosis intervention performance issues in real time and to overcome the issues commonly faced when monitoring progress in early diagnosis. I look forward to updating you on the findings of this research in a future blog post!

The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorse those views or opinions.

Leave a Reply