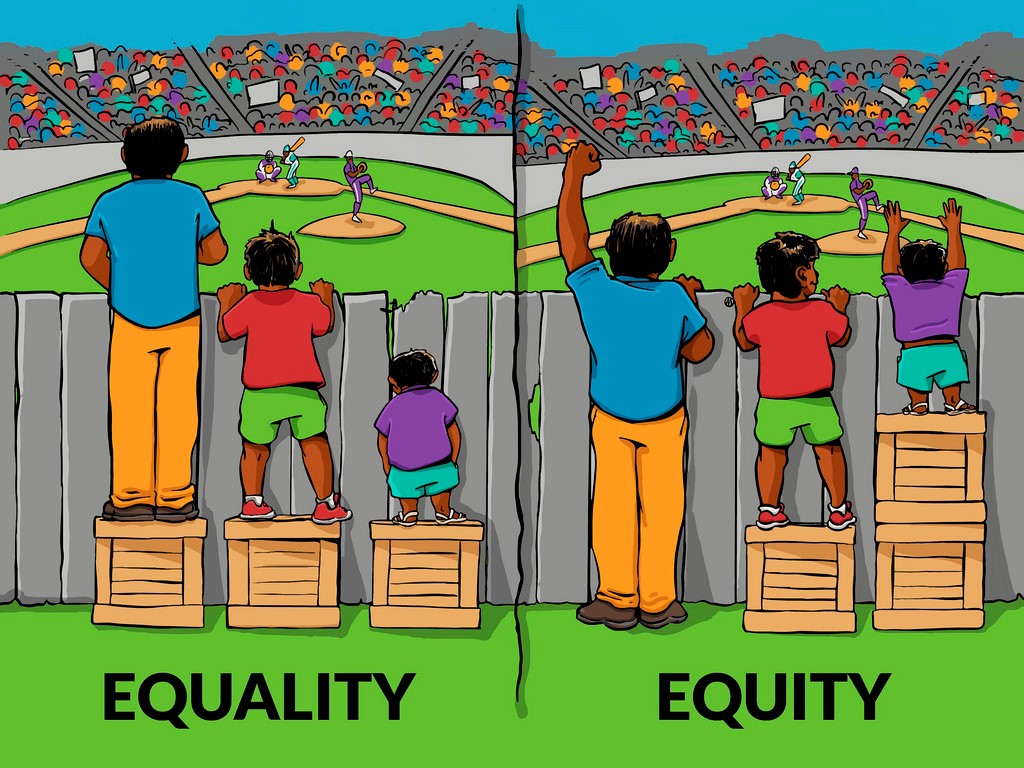
The classic American illustration explaining the difference between equity and equality is of three people trying to watch a baseball game from behind a fence. In the first picture three people all stand on an equal sized box. This represents equality, but because the three people are of very different heights only two of them can see over the fence. In the second picture, the tallest man stands on the ground and the shortest has two boxes to stand on. In this picture, representing equity, all three can watch the game. Although the distribution of boxes in unequal, it is fair because everyone is given what they need to enjoy the game.
Cancer screening aims reduce cancer mortality in the population. Ideally it will also succeed in reducing health inequalities in society. It can often achieve this by targeting the whole population and it is those who generally have least access to good health care who may benefit most from screening.
Economists talk about two types of equity. Horizontal equity refers to a taxation system under which people with equal means pay the same tax. That is the sort of equity that screening programmes have tried to achieve so far: those with equal need for screening should be equally likely to receive screening. Vertical equity goes further: it refers to taxation systems in which those with greater means contribute more through their taxes. Although rarely made explicit in the definition of vertical equity, those who earn more should not simply pay more in taxes, but they should pay a higher rate of taxes. In a commentary in the Lancet Gastroenterology & Hepatology, I ask what should a screening programme that aims to achieve vertical equity look like.
As a public health intervention, population screening targets everyone (often identified by age and sex) equally regardless of their risk. In practice, many screening programmes are less successful attracting individuals from certain ethnic groups and individuals who are more deprived or less well educated. To promote horizontal equity, screening programmes should include elements to promote equity (e.g., providing information in braille and formats suitable for people with learning difficulties), but traditionally despite aiming to reduce inequalities it is mostly a case of “one-size fits all”.
Consider bowel screening using FIT (faecal immunochemical test). Unlike many previous screening tests, FIT measures the amount of blood in stool and so it is necessary to consider at what level the test should be called positive. In the name of vertical equity, one may ask whether different thresholds should be used for different people. If we want to personalise the threshold, how should it be done equitably? It doesn’t seem like a difficult question until you start going in to details.
At all ages, women have lower rates of bowel cancer than men. So, in the interest of equity, should we not offer screening from a younger age to men than women? On the other hand, women with bowel cancer tend to have a lower score on FIT than men, so to be equitable (in terms of detecting a equal proportion of cancers at an early stage) should we call a test positive at a lower level for women than men?
There are many ways to define what is equitable and the way in which we design our screening programmes depends critically on what it is we are aiming to achieve. Which of the following do you think should be considered equitable?
- Having equal risk of dying from colorectal cancer in the next 10 years
- Reducing the risk of dying from colorectal cancer in the next 10 years by the same amount
- Reducing the risk of dying from colorectal cancer in the next 10 years by the same proportion
- Detecting the same proportion of colorectal cancers on screening
- Having equal chance of having colorectal cancer diagnosed between screens
- Being equally likely to have colorectal cancer found if you test positive on screening
- Gaining the same health benefit by participating in screening.
The last of these is often used in health resource allocation and is formalised using a measure called QALYs (Quality Adjusted Life Years). The difficulty in using QALYs to determine who to invite for screening is that one would be less likely to invite those who are most health deprived. Blind people and people in wheelchairs have a reduced quality of life so that if thanks to screening they live an additional 20 years, they will gain fewer QALYs than someone who has no such disability. Similarly, someone with a shorter life expectancy will gain fewer QALYs if they are prevented from dying from colorectal cancer thanks to screening than someone with a longer life-expectancy.
In the Commentary, I argue that whereas population-level decisions about screening will most likely continue to be made based on QALYs, decisions regarding individualisation of screening should be based on equalising risk. People should be invited based on their risk of having a screen-detected early-stage cancer; referral to a specialist should be based on equal risk of having cancer; and the date of the next screen should be based on trying to equalise the risk of having a late-stage cancer found before or on the next screen.
Over the last decade, the debate about medical screening has focused on estimating and communicating harms as well as benefits of screening. Over the next decade, you will hear far more about equity.
The views expressed are those of the author. Posting of the blog does not signify that the Cancer Prevention Group endorse those views or opinions.
Share this page

Leave a Reply