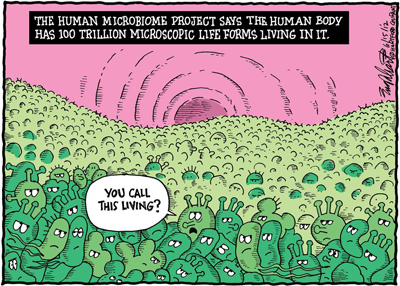
It might surprise you that your body is made up of only 10% human cells. There are trillions of microscopic creatures living and dying all over you, and these are particularly diverse and numerous in the human gut. Mounting evidence suggests that microbes aren’t all enemies but are vital to our functioning, influencing our metabolism, health, behaviour, and quality of life. The deep collaboration between humans and their commensal microbes is the focus of much new research that invites us to think about ourselves differently. This article looks at some of the bold claims made from this young field.
The genomes of our microbiota, and the way they interact with the human host, are collectively termed the microbiome. Novel genomic technologies have enabled microbiology to move beyond previous constraints: previously, researchers had to isolate individual species in cultures and study them in sterile labs; now, we can gather microbial samples directly from faecal samples, and extract and analyse the full DNA complement. We can also start to unpick their functions.
Functions of the microbiome
The importance of the gut flora for human health is increasingly recognised, to the extent that microbiome modification has been proposed by some as a potential therapeutic treatment. Microbes are involved in considerable co-meta bolism with their hosts (humans), producing some vitamins that we alone do not have the genes to synthesize, as well as breaking down food to extract nutrients that provide an important component of our calorific intake. This direct impact of microbes upon the energy content of the human diet links the gut microbiome to the development of the human immune system, and abnormalities in microbial diversity are correlated with several inflammatory diseases, colon cancer, diabetes, and obesity (1).
bolism with their hosts (humans), producing some vitamins that we alone do not have the genes to synthesize, as well as breaking down food to extract nutrients that provide an important component of our calorific intake. This direct impact of microbes upon the energy content of the human diet links the gut microbiome to the development of the human immune system, and abnormalities in microbial diversity are correlated with several inflammatory diseases, colon cancer, diabetes, and obesity (1).
Research on microbiome functions has recently taken a surprising turn – it seems that microbes might also be able to ‘talk to’ our brain and influence mood and behaviour. The idea behind the ‘gut-brain axis’ is that microbial cultures interact with nervous systems through the molecules and proteins they secrete. This idea is more intuitive when we consider that gastro-intestinal problems and psychiatric symptoms (such as anxiety and autism) commonly co-occur (2). Can we trust the bold claims made based on the research so far?
Can microbes explain psychiatric symptoms? Some exciting research has found that alteration of the gut microbiome contributes to some of the behavioural abnormalities displayed in a mouse model of autism (3). One trial of an extended faecal microbiota transplant in 18 autism-diagnosed children found an 80% reduction of gastro-intestinal symptoms at the end of treatment (4). But these studies are extremely limited, making it very difficult to draw solid conclusions about a causal role for specific bacteria in autistic disorders, which are complex neurobiological phenomena. Can the germ-free mice used in the former study possibly be informative given the real-world diversity of the human microbiome? Alarmingly, the microbiota transplant (‘poo pill’) trial had no placebo controls. Even more alarmingly, their pills are already a patented autism treatment (https://www.google.com/patents/US20160339065). A more convincing trial in humans tested for emotional and physiological effects of prebiotics (these are bacterial food sources that cannot be metabolised by the host organism, while probiotics are live microorganisms) on a small group of human volunteers. They found that participants who were given a prebiotics course had lowered levels of salivary cortisol (a stress-related hormone), and showed decreased attention towards negative stimuli, as measured by Attentional Dot-Probe and facial expression recognition tasks (5). But this study was funded by the biotech company that sells prebiotics, including the one used in the trial, which is worrying given their incentive to legitimise an extremely marketable treatment and an extremely simplified explanation for neuropsychiatric problems like depression and anxiety.
To sum up, more (and better) research is needed. We are very far from determining precisely how different bacteria influence the brain via the immune, metabolic and nervous systems. The existing evidence is quite preliminary and not causal, so the connections to disorders like autism and anxiety are a bit of a stretch and are worryingly oversimplified in the media. What’s more, it is difficult to tease apart confounding factors e.g. diet, home lives, other enviromental exposures, which all affect an individual’s microbiota and development. Everyone has a unique and constantly changing microbiome – we can’t prescribe a “one size fits all” microbiome treatment. A lot of the hype is probably driven by the money-spinning industries of food, supplements and pharmaceuticals. We’ve seen a shift from one extreme to another – from condemning ‘bad bacteria’ to ‘microbiomania’. It’s clear that we’re in deep symbiosis with our microbes, let’s not label them!
image 1 from http://learn.genetics.utah.edu/content/microbiome/changing/
image 2 from http://medicine.emory.edu/research/interest-groups-research-teams/microbiome/
Bibliography
- Rauch M, Lynch SV. The potential for probiotic manipulation of the gastrointestinal microbiome. Curr Opin Biotechnol. 2012 Apr;23(2):192–201.
- Cryan JF, Dinan TG. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci. 2012 Oct;13(10):701–12.
- Hsiao EY, McBride SW, Hsien S, Sharon G, Hyde ER, McCue T, et al. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell. 2013 Dec 19;155(7):1451–63.
- Kang D-W, Adams JB, Gregory AC, Borody T, Chittick L, Fasano A, et al. Microbiota Transfer Therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study. Microbiome. 2017 Jan 23;5(1):10.
- Schmidt K, Cowen PJ, Harmer CJ, Tzortzis G, Errington S, Burnet PWJ. Prebiotic intake reduces the waking cortisol response and alters emotional bias in healthy volunteers. Psychopharmacology (Berl). 2015 May;232(10):1793–801.


[…] research has not yet reshaped our conceptions of mental health etiology and treatment (see my previous article), but it should be causing havoc in the social sciences – particularly for anthropologists, who […]